Lien resolution is often an overlooked step in the settlement process. Nonresponsive lienholders, incomplete billing records, and the pressure to close a case quickly can easily push lien resolution to “tomorrow’s” to-do list. But delaying this step can have serious consequences – reducing the client’s net recovery and increasing the attorney’s potential risk exposure.
Handled incorrectly, liens can delay settlements, reduce client satisfaction, or even open the door to malpractice claims. Handled properly, they protect all parties, maximize recovery, and close cases with confidence.
That’s where ClearLiens by Medivest comes in. Our comprehensive lien resolution services are designed to help attorneys avoid common mistakes, stay compliant, and ensure clients receive the best possible outcomes. To illustrate why lien resolution matters so much, here is a list of five common mistakes attorneys make during the lien resolution process and how to avoid them.
1. Waiting Too Long to Address Liens
Mistake: Many attorneys focus on negotiating the best settlement first, leaving liens as an afterthought.
Risk: Liens don’t go away simply because a settlement is reached. Ignoring them until the end can stall settlement disbursement, leave attorneys scrambling to resolve last-minute issues, or even trigger accrued interest for the client due to failing to pay liens on time (Medicare).
Avoid Problems: Start identifying potential lienholders as early as possible by doing a lien investigation. Building lien resolution into your case workflow ensures there are no surprises when it’s time to disburse funds.
2. Failing to Identify All Liens Properly
Mistake: Overlooking certain lienholders, particularly government entities like Medicare, Medicaid or the Department of Veterans Affairs (VA), Medicare Advantage Plans (MAPs) Managed Care Organizations (MCO’s which are privately administered Medicaid), or any other private health insurance creates hidden risks.
Risk: Missing a lien can expose attorneys and clients to unforeseen repayment obligations, and for Medicare liens, heavy interest obligations, or even double damages. In some cases, the amount of an undiscovered lien can even exceed the settlement itself, leaving the client and, more likely, the attorney with a significant hurdle to overcome.
Avoid Problems: Implement a thorough intake and verification process to minimize potential issues. Ask clients detailed questions about their insurance coverage and treatment history, and confirm with all potential lienholders before closing the case.
3. Accepting the First Payoff Amount Without Question
Mistake: Paying whatever amount the lienholder initially demands.
Risk: Many lien demands include unrelated charges or fail to account for reductions due to case-specific factors, such as comparative fault or limited policy limits. Paying in full without review can unnecessarily reduce your client’s net recovery.
Avoid Problems: Always request an itemized statement and review the detailed payment spreadsheet carefully. Challenge unrelated or inflated expenses and negotiate reductions. Lienholders are often willing to compromise when presented with evidence of financial hardship, pre-existing medical conditions, or legal grounds for reduction.
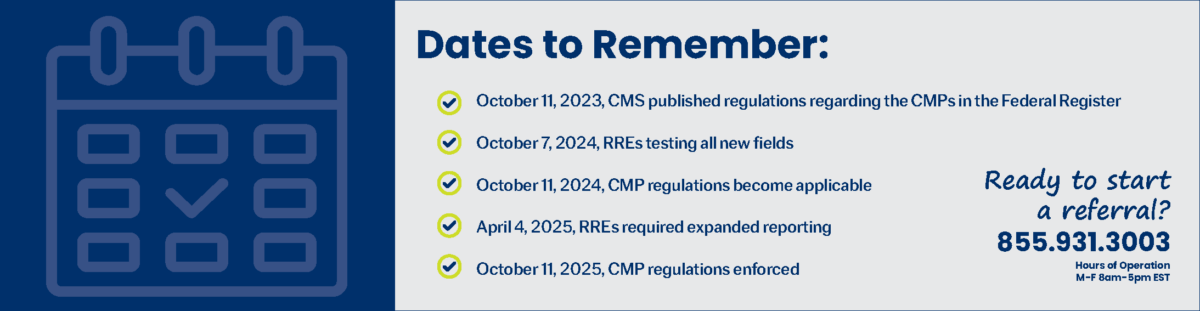
4. Ignoring Compliance Requirements (Especially Medicare)
Mistake: Skipping or mishandling compliance obligations, such as reporting to the Centers for Medicare & Medicaid Services (CMS).
Risk: Failing to follow Medicare’s strict notification and repayment timelines can result in significant interest obligations or potential penalties, and can create unnecessary liability for your firm.
Right of Action Against “Any Entity”
- The MSP statute gives Medicare the right to pursue recovery from any party that paid the claim or received a portion of the settlement funds as well as providers who received payment for services related to the compensated claim. This includes the claimant, attorneys, and even insurers in some cases.
Double Damages Penalty
- If Medicare has to take legal action to recover, the statute allows it to seek double its damages (the amount it paid conditionally minus procurement costs), plus interest.
Avoid Problems: Treat Medicare compliance as a non-negotiable requirement. Familiarize yourself with CMS guidelines or partner with a professional lien resolution provider, such as Medivest, to ensure all requirements are met accurately and on time.
5. Ignoring Compliance Requirements (Especially Medicare Not Educating Clients About Liens Obligations and Timelines)
Mistake: Waiting until after settlement to explain lien obligations and the time it may take to resolve them.
Risk: Clients are often surprised to learn that a significant portion of their settlement will be directed toward healthcare liens. Even more frustrating, lien resolution is not always a quick process. While some liens can take as little as 60 days, others may stretch close to a year, depending on the complexity and the responsiveness of the lienholder. This lack of transparency can leave clients feeling blindsided, dissatisfied, and distrustful, which may lead to strained relationships or even formal complaints.
Avoid Problems: Set clear expectations with clients from the start. Explain both the financial impact of liens and the possible timelines for resolution. By discussing upfront that lien resolution is a necessary, and sometimes lengthy, part of the process, you build trust, manage expectations, and help clients stay patient and informed while waiting for their settlement funds to be finalized.
Conclusion: Protecting Clients, Protecting Your Practice
Lien resolution is far more than a box to check at the close of a case. It’s a critical component of risk management and client advocacy. By addressing liens properly and avoiding common mistakes, attorneys can maximize client recoveries, reduce delays, and protect themselves from unnecessary liability.
If lien resolution feels overwhelming or time-consuming, you don’t have to handle it alone. ClearLiens by Medivest, specializes in navigating the complexities of Medicare, MAP, Medicaid, MCO, VA, TriCare, FEHBA/FELA, ERISA, Hospital/Private Healthcare, and other healthcare-related liens. Partnering with our team helps ensure compliance, streamlines the resolution process, and safeguards both your clients and your practice.
For questions or to get started on a case today, visit us here to request more information.