Consider this scenario: you are a personal injury attorney, and you get a call from a new client who is 63 years old and is interested in settling her automobile accident case. Per the Medicare Secondary Payer statute and as part of the case workup, you need to make sure you are not shifting the burden to Medicare.
What is the Medicare Secondary Payer Statute?
The MSP statute was passed by Congress in 1980 in order to protect the financial integrity of the Medicare Trust Fund. Per this statute/law, Medicare is a secondary payer for workers’ compensation, no-fault insurance, liability insurance, self-insured plans, and employer group health plan insurance. According to the MSP regulations, these other sources of health care coverage are to be the primary payer, with Medicare being the secondary form of payment.
What is a Medicare Set-Aside (MSA) Proposal?
A MSA proposal is a detailed report indicating the anticipated Medicare allowable, Injury-related expenses for the remainder of the injured individual’s life expectancy. It is a calculation that determines a dollar amount that should be “set aside” as part of the settlement process to satisfy the Medicare Secondary Payer Statute (MSP) and to avoid shifting the burden to Medicare.
Guidance from Medicare for Liability Cases
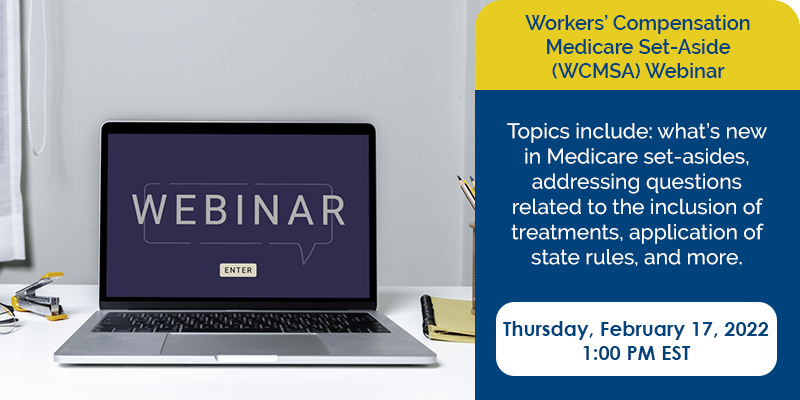
The Centers for Medicare and Medicaid Services (CMS) published the WCMSA Reference Guide to help attorneys understand the process CMS uses for approving proposed Workers’ Compensation MSA (WCMSA) arrangements. The purpose of the WCMSA Reference Guide was to consolidate and supplant all the historical CMS memos into a single point of reference.
However, Workers’ Compensation and Liability settlements have several different nuances. CMS has yet to release the long-awaited LMSA Reference Guide for liability settlements, despite announcing its intention to do so in 2018. Given the current lack of guidance concerning Liability MSAs from CMS, attorneys should look to the WCMSA Reference Guide for guidance when settling their liability cases.
Litmus Test – Is a MSA Proposal Recommended?
In order to determine if a MSA allocation is recommended to cover Medicare’s interest in your settlement, there are several key items to review. Attorneys can do a quick MSA litmus test to determine whether or not a MSA is recommended.
-
Your client is currently Medicare-eligible
-
Your client is 62.5 years old and within 30 months of becoming eligible for Medicare benefits
-
Your client has either applied for Social Security Disability Insurance (SSDI) or has an open or pending application Will there be any money after medical liens have been resolved to fund a Medicare Set-Aside (MSA) account?
Medicare Eligibility
What is Medicare’s criteria for an individual to become Medicare eligible? Medicare is available for people aged 65 or older, younger people with disabilities, and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant).
Social Security Disability Insurance (SSDI)
An individual who has either applied or has reapplied for Social Security Disability Insurance can become Medicare eligible. Social Security Disability Insurance (SSDI) is a federal program that helps those who have become disabled from work. An individual can apply for SSDI when:
-
A person is unable to engage in any “substantial gainful activity” due to an illness or disability and;
-
When a person is not able to return to work for 12 months or more and;
-
When a person has accumulated enough work credits in the last 10 years to qualify.
30 Months to Become Medicare Eligible
The reason why it takes 30 months to become Medicare eligible after the individual has either applied or reapplied for SSDI is that:
-
The individual needs to wait one month after the date of injury to apply for SSDI.
-
After the SSDI applicate date, there is a waiting period of 5 months to receive SSDI entitlement.
-
From the date of SSDI entitlement, Medicare has 24 months waiting period to become Medicare eligible.