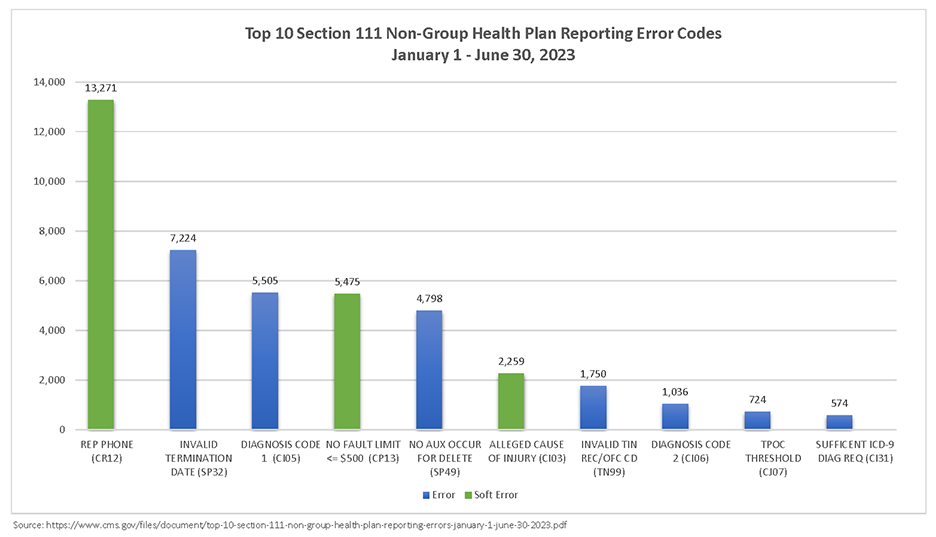
On June 5, 2023 Centers for Medicare & Medicaid Services (CMS) updated the MMSEA Section 111 NGHP User Guide version 7.2. It has been posted to the NGHP User Guide page on CMS.gov. The NGHP User Guide version 7.2 replaces Version 7.1 which was released on April 4, 2023.
To download the updated MMSEA Section 111 NGHP User Guide 7.2 click here.
Who Must Report
An organization that must report under Section 111 is referred to as a responsible reporting entity (RRE). In general terms, NGHP RREs include liability insurers, no-fault insurers, and workers’ compensation plans and insurers. RREs may also be organizations that are self-insured with respect to liability insurance, no-fault insurance, and workers’ compensation.
What’s New – 7.2 Version
New information regarding Mandatory Insurer Reporting for Non-Group Health Plans (NGHPs) and NGHP Town Hall Events is posted here as it becomes available.
MMSEA III – June 6, 2023 – NGHP User Guide 7.2 Version Updates
-
- Chapter I: Introduction and Overview
- Chapter II: Registration Procedures
- Chapter III: Policy Guidance
- Chapter IV: Technical Information
- Chapter V: Appendices
- 270/271 Health Care Eligibility Benefit Inquiry and Response Companion Guide for Mandatory Reporting NGHP Entities, Version 5.8
-
Chapter I: Introduction and Overview – Updates
The updates listed below have been made to the Introduction and Overview Chapter Version 7.2 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide as necessary. There are no version updates to this chapter.
-
Chapter II: Registration Procedures – Updates
The update listed below has been made to the Registration Procedures Chapter Version 7.2 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide as necessary. There are no version updates to this chapter.
-
Chapter III: Policy Guidance – Updates
The updates listed below have been made to the Policy Guidance Chapter Version 7.2 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide as necessary. The guidance on determining the ORM termination date based on a physician statement has been clarified (Section 6.3.2). Guidance on what triggers the need to report ORM has been clarified (Sections 6.3 and 6.5.1.1).
-
Chapter IV: Technical Information – Updates
The updates listed below have been made to the Technical Information Chapter Version 7.2 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide, as necessary. The NGHP Unsolicited Response File format has been simplified, and filename formats have been added (Section 7.5 and Chapter 10). For liability claims, it is now optional to report ‘NOINJ’ codes in certain circumstances (Section 6.2.5.2).
-
Chapter 5: Appendices – Updates
The updates listed below have been made to the Appendices Chapter Version 7.2 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide as necessary. The end-of-line character has been clarified for files using HEW software (Appendix E). The NGHP Unsolicited Response File layout has been simplified (Appendix F).
-
270/271 Health Care Eligibility Benefit Inquiry and Response Companion Guide for Mandatory Reporting NGHP Entities, Version 5.8 – Changes for this Release
The updates listed below have been made to the Appendices Chapter Version 7.2 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide as necessary. The end-of-line character has been clarified for files using HEW software (Appendix E). The NGHP Unsolicited Response File layout has been simplified (Appendix F).
For Additional Information
Medivest will continue to monitor changes occurring at CMS and will keep its readers up to date when such changes are announced. For questions, feel free to reach out to the Medivest representative in your area by clicking here or call us direct at 877.725.2467.