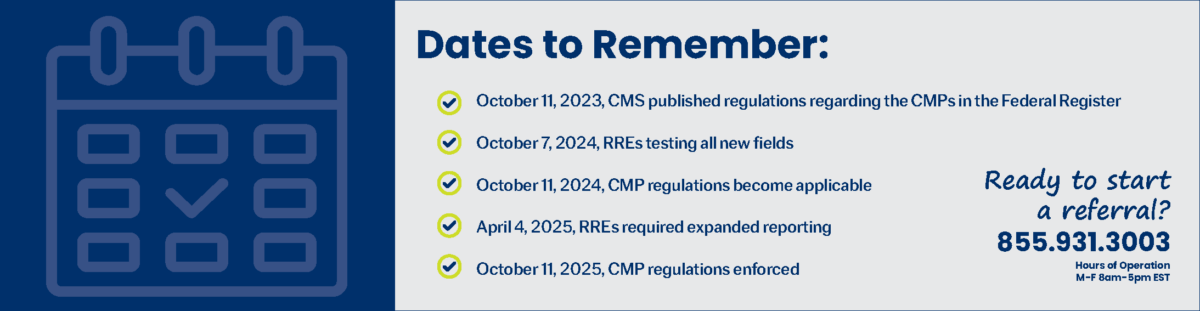
On October 7, 2024, the Centers for Medicare & Medicaid Services (CMS) updated the MMSEA Section 111 NGHP User Guide to version 7.7. It has been posted to the NGHP User Guide page, found here. The NGHP User Guide to version 7.7 replaces Version 7.6 which was released on July 2, 2024.
MMSEA III – October 7, 2024 – NGHP User Guide Downloads 7.7
Updates: The updates listed below have been made to the Introduction and Overview Chapter Version 7.7 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide as necessary. The table describing system-generated emails has been updated to include information for the RRE ID Notification email that is sent once a user completes the initial registration function and the Successful Registration PIN email that is sent once vetting is successful on the Section 111 COB Secure Website (COBSW) (Table 7-1).
Updates: The update listed below has been made to the Registration Procedures Chapter Version 7.7 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide as necessary. The table describing system-generated emails has been updated to include information for the RRE ID Notification email that is sent once a user completes the initial registration function and the Successful Registration PIN email that is sent once vetting is successful on the Section 111 COB Secure Website (COBSW) (Table 6-4).
Updates: The updates listed below have been made to the Policy Guidance Chapter Version 7.7 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide as necessary. For clarification, a note has been added to indicate that settlements, judgments, awards, or other payments obtained entirely under the wrongful death theory of liability, which do not claim and release medicals, or have the effect of releasing medicals, are not required to be reported (Section 6.5.1.4).
Updates: The updates listed below have been made to the Technical Information Chapter Version 7.7 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide, as necessary. For NGHP claim files, a new “04” warning flag will be applied to claim response files with open ORM records when the later date of either the CMS Date of Incident on the claim record or the Part A Add Date is greater than 135 calendar days from the Start Date of the RRE’s submission period. Additionally, compliance flag fields have been renamed warning flag (Sections 6.1 and 6.9.1 and Chapter 7). The table describing system-generated emails has been updated to include information for the RRE ID Notification email that is sent once a user completes the initial registration function and the Successful Registration PIN email that is sent once vetting is successful on the Section 111 COB Secure Website (COBSW) (Table 12-1). The description of Response File disposition code 03 has been clarified (7.1).
Updates: The updates listed below have been made to the Appendices Chapter Version 7.7 of the NGHP User Guide. As indicated on prior Section 111 NGHP Town Hall teleconferences, the Centers for Medicare & Medicaid Services (CMS) continue to review reporting requirements and will post any applicable updates in the form of revisions to Alerts and the user guide as necessary. For NGHP claim files, a new “04” warning flag will be applied to claim response files with open ORM records when the later date of either the CMS Date of Incident on the claim record or the Part A Add Date is greater than 135 calendar days from the Start Date of the RRE’s submission period. Additionally, compliance flag fields have been renamed warning flag (Appendix C and Appendix G). The description of Response File disposition code 03 has been clarified (Appendix G).
Changes for This Release: The email address for contacting an Electronic Data Interchange (EDI) Representative has changed to COBVA@bcrcgdit.com. However, COBVA emails coming from CMS now show the address as COBVA@mail.cms.hhs.gov (Customer Support).
For Additional Information
Medivest will continue to monitor changes occurring at CMS and will keep its readers up to date when such changes are announced. For questions, feel free to reach out to the Medivest representative in your area by clicking here or call us direct at 877.725.2467.