On November 13, 2023, CMS hosted a previously announced webinar focused on its upcoming expansion of Total Payment Obligation of Claimant settlement data (TPOC) to be reported under the Medicare Secondary Payer statute’s (MSP) Section 111 Mandatory Insurance Reporting.
The additional TPOC settlement data to be reported specifically includes whether a WCMSA amount was established and if so, any amount above $0.00 so designated, the amount that was approved by CMS (if applicable), the period of coverage (i.e. life expectancy of the injured worker), the funding type – whether funded by lump sum or via a structured annuity (without commenting on any preference or presumptions by CMS if funded one way or another), if funded by structure, the seed amount (a type of down payment estimating the first two years of coverage plus initial surgery for any included body part(s), the anniversary deposit (when additional annuitized payments would be made), the Case Control Number (starts with a W if submitted to CMS for approval or a 0 or 1 if not submitted), and the Professional Administrator’s EIN.
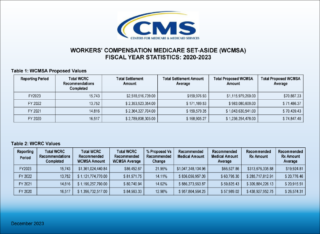
The premise for including the additional WCMSA information with TPOC data is to allow CMS to flag injury related medical diagnosis codes (ICD codes) in the Medicare beneficiaries’ record called the Common Working File (CWF) with a “W” (at least for those WCMSA’s that have been approved) to assist CMS in being more efficient at denying payment for medicals that are injury related and compensated in the TPOC settlement. The Workers’ Compensation (WC) carriers or self insureds appoint Responsible Reporting Entities (RREs) to currently provide Section 111 data for both ongoing claims with Ongoing Responsibility for Medicals (ORMs) and for settlements (TPOCs). Under this expanded reporting data set, RREs would be expected to submit this information for then current Medicare beneficiaries, with testing to occur in 2024 and implementation projected to begin in early 2025 as early as January 2025. While presenter John Jenkins, CMS Health Insurance Specialist, who also presented for CMS when the addition of Section 4.3 in the Workers’ Compensation Medicare Set-Aside Reference Guide (WCMSA Reference Guide) was announced and when CMS modified that language, made it clear that this expanded reporting expectation would not extend to No Fault or liability settlements compensating for future medicals (i.e. NFMSA’s or LMSA’s), he did say it was intended to cover WCMSA TPOC information even if the WCMSA at issue was not submitted to CMS for review/approval. For example, if the WCMSA allocation report used an Evidenced Based Medicine cost projection Method or other non-submit projection method as opposed to a CMS cost projection methodology espoused under the WCMSA Reference Guide, Jenkins explained that there would still be an expectation that this additional data would be reported to CMS.
Jenkins also indicated that once the WCMSA information is reported under Section 111, notification would be sent to the Medicare beneficiary directly.
As background in describing the history of Section 111, Jenkins reminded listeners that Section 111 is part of the federal MSP statute (42 U.S.C. Section 1395y(b)(2) et seq., and that its provisions were added to the MSP pursuant to the 2007 Medicare and Medicaid SCHIP Extension Act (MMSEA)(implemented a few years later). He also pointed out that in addition to the federal MSP statute, the regulations to the MSP are found in the Code of Federal Regulation (CFR) and that 42 C.F.R. 411.46 specifically, reiterates Medicare as a secondary payer to Workers’ Compensation claims (including for both ORM and TPOC’s, and that nothing in the webinar would replace any existing requirements of Responsible Reporting Entities as to thresholds for reporting ORM or TPOC’s).
Answers to questions from the webinar audience were provided by both Steve Forry, CMS Director Division of MSP Program Operations and presenter, John Jenkins, CMS Health Insurance Specialist.
Questions regarding the webinar’s contents and the subject matter may be submitted to CMS via its dedicated Section 111 email address, s111WCMSA@cms.hhs.gov.
Take Aways
This webinar gives us a glimpse as to how CMS intends to address the EBM and other non-submit WCMSA’s that it originally referenced when it added Section 4.3 to the WCMSA Reference Guide. How CMS will be able to require data for something that is not required by law was not elaborated on and is yet to be seen. However, as we in the MSP industry have always understood, while the WCMSA submission process is and has always been voluntary, we always knew that if you submit for approval, you are essentially now in the CMS arena where you will be playing by its guidance/rules. Now, even if you don’t submit a WCMSA for approval, ostensibly for your RRE to be able to complete the Mandatory Insurance Reporting under Section 111, it seems the WCMSA amount and other new data will be available for CMS to assist it in its quest to comply with the MSP and prevent Medicare from paying until the primary plan’s injury related future compensation has been exhausted.
Claimant attorneys should be made aware of this procedure at the time it is implemented so they can field questions that may come back to them by injured workers. Likewise, adjusters handling WC claims may also get follow up calls asking for clarification and what the notification means. Ultimately, this means that representatives for WC carriers and representatives for injured workers should solidify their methods of providing informed consent to their respective clients so that nobody is surprised when a post settlement injury related medical that is usually Medicare covered is denied. For those who establish WCMSA’s, the solution is to bill the WCMSA, document the expenditure (with items and services priced at the respective fee schedule rate and the prescription drugs at Redbook Average Wholesale Price (AWP), and keep up with attestations to CMS on an annual basis so that once exhausted, Medicare would become primary.
What’s New?
A new coversheet is available for any Non Group Health Plan (NGHP) or agent when corresponding with the Commercial Recovery Center (CRC) and can be found here: CRC NGHP Correspondence Cover Sheet (cms.gov)
The NGHP Appeals Quick Reference Guide was updated and is available here: NGHP Submit Appeals Quick Reference Guide April 2023 (cms.gov)
For Additional Information
Count on Medivest to help keep you up to date with the constant updates, guidance, and rule changes related to CMS’s enforcement of the MSP on a regular basis. For questions, feel free to reach out to the Medivest representative in your area by clicking here or call us direct at 877.725.2467.