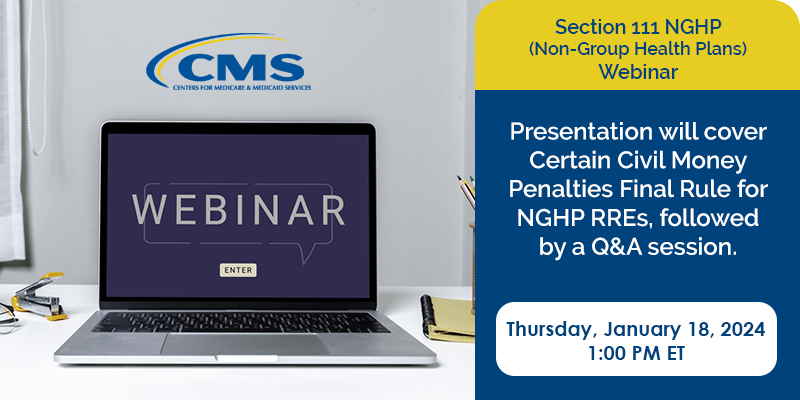
On Tuesday April 16, 2024, Centers for Medicare & Medicaid Services (CMS) will be hosting a second webinar regarding the expansion of Section 111 Non-Group Health Plan (NGHP) Total Payment Obligation to Claimant (TPOC) reporting to include Workers’ Compensation Medicare Set-Aside (WCMSA) information. After the first webinar in November, CMS received additional questions and feedback from the industry. The intent of this webinar is to ensure that RREs will be prepared for the change once implemented.
With that in mind, this webinar will include a background recap, summary of technical details, updated timelines and CMP impacts. The presentation will be followed by a question and answer session. Because this expansion impacts reporting of WCMSAs, it is strongly recommended that Responsible Reporting Entities (RREs) that report Workers’ Compensation settlements attend.
Date: April 16, 2024
Time: 2:00 PM EST
Webinar Link: https://cms.zoomgov.com/s/1610015349?pwd=NHcza3NhcDlCdjM0cVhENWlNcFBjZz09
Passcode: 750766
Or to connect via phone:
Conference Dial In: 1-833-568-8864
Conference Passcode: 161 001 5349
Additional information about the most recent updates from CMS can be found here. If you have questions on how topics discussed in this webinar may affect your clients or your company, please contact Medivest or call us at 877.725.2467.